PERSISTENT
COUGH
PERSISTENT
COUGH
SHORTNESS
OF BREATH
SHORTNESS
OF BREATH
OF BREATH
FATIGUE
FATIGUE
If you have these common respiratory symptoms and are struggling to find an accurate diagnosis, you’re probably feeling confused and frustrated.
A rare lung disease may be the cause.
Pulmonary alveolar proteinosis (PAP) is a lung disease that's hard to diagnose and often misdiagnosed. This is because its symptoms are also common to other respiratory illnesses like pneumonia, bronchitis, and asthma.
Do you have respiratory symptoms that
won't go away, even after treatment?
Common signs and symptoms
(including difficulty climbing stairs, walking)
(weight loss or weight gain due to limited activity)
If you've experienced any of these symptoms with no relief from treatment, and your doctor has mentioned unusual patterns in your lung scans—it may be time to talk to them about PAP.
What is PAP?
Pulmonary alveolar proteinosis (PAP) is a lung disease in which a substance called surfactant builds up in the lungs. Surfactant is a substance that may have an oily, mucus-like consistency. When surfactant builds up, it’s hard to breathe.
Types of PAP
- Primary PAP: Caused by a disruption to specific white blood cells in your lungs that causes them to not work properly. This can fall into two categories:
- Autoimmune PAP (aPAP)
- Hereditary PAP
- Secondary PAP: Caused by another disease (such as myelodysplastic syndrome or chronic myelogenous leukemia), certain infections, and potentially harmful toxins when inhaled (such as silica and talc)
- Congenital PAP: The least common type of PAP and is the result of a genetic mutation, which occurs at birth
In the United States, about 7 in 1 million people are diagnosed with PAP.
However, because many doctors are not familiar with PAP, they don’t even know to test for it—making the true number of PAP cases unknown.
Autoimmune PAP (aPAP) is the most common form of PAP, accounting for about 90% of PAP cases.
In aPAP, the immune system mistakenly targets the protein that activates the cells needed to keep the lungs clear.
Because aPAP is a disease with symptoms that mimic more common respiratory conditions, it can take an average of 18 months from the time a person starts to feel symptoms to be diagnosed.
Although symptoms of aPAP can appear as early as childhood, most people are diagnosed in their 30s to 50s. It’s not more common in any sex, race, or region of the world. Studies suggest that smoking and exposure to fumes may contribute to an increased risk, but these are not always factors in people who are diagnosed.
How does aPAP affect you?
In aPAP, some white blood cells in the air sacs of the lungs (the alveoli) don’t work properly.
For these cells to work correctly, they need a special protein called granulocyte-macrophage colony-stimulating factor (GM-CSF). But in aPAP, the body mistakenly blocks GM-CSF from binding to the white blood cells, preventing them from doing their job. As a result, surfactant—a substance with an oily, mucus-like consistency—builds up, which makes it hard to breathe. This blocking is caused by antibodies produced by the immune system, called GM-CSF autoantibodies.
A simple blood test can detect these GM-CSF autoantibodies to confirm or rule out aPAP. However, since many pulmonologists aren't familiar with testing for aPAP specifically, they may suggest these other tests first. These tests are more invasive and may require hospitalization.
Bronchoscopy
In a bronchoscopy, a doctor is able to see inside and examine a patient’s lungs and airways by passing a thin tube through the nose or mouth.
Biopsy
A biopsy may be performed by removing lung tissue or cells from the body. This can be done with a special needle or through surgery in an operating room.
How to rule out or confirm aPAP
Savara sponsors a no charge, third-party testing program to reduce barriers to GM-CSF autoantibody testing. This program can also provide you and your healthcare professional with more information about how testing may be used as a diagnostic resource to help confirm or rule out aPAP and potentially reduce delays in diagnosis. Neither you, your healthcare provider, nor your health insurance provider will be billed for this program.
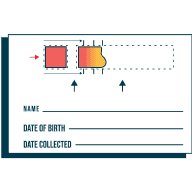
One simple test
Through the aPAP ClearPath™ Testing Program, a simple, accurate, and noninvasive blood test can help confirm or rule out autoimmune pulmonary alveolar proteinosis (aPAP).
This blood test is available for your doctor to order in 1 of 2 forms:
Serum-based test:
Dried blood spot test:
Healthcare professionals and patients who use this program have no obligation to recommend, purchase, order, prescribe, promote, administer, use, or support any Savara product.
The aPAP ClearPath™ Testing Program is not intended to and should not interfere in any way with your healthcare professional’s or your independent judgment and choice in the management options for aPAP. Healthcare professionals and patients should always consider the full range of management options and select those most appropriate for the individual patient.
Living with aPAP
Living with aPAP can be challenging. These patients talk through their journeys with the disease and how they're learning to navigate their lives after being diagnosed.
Meet Kelsea. An avid gardener who didn't know anything was wrong until doctors discovered low oxygen levels.
"It's difficult because a lot of people don't understand it."
-Kelsea
Meet Niki. An active athlete who started to notice shortness of breath and persistent coughing.
"You realize your vulnerability. You realize the delicacy of life. You realize that you're not invincible."
-Niki
Meet Eric. A personal trainer who found the right specialist at the right time.
"The pulmonologist at the hospital I was at didn't know anything about aPAP. Zero."
-Eric
Hear Eric and his doctor discuss his journey with aPAP.
"Had Eric undergone blood testing for suspected autoimmune PAP, the lung biopsy and subsequent infection and hospitalization would have been avoided."
-Bruce C. Trapnell, MD
Meet Kelsea. An avid gardener who didn't know anything was wrong until doctors discovered low oxygen levels.
"It's difficult because a lot of people don't understand it."
-Kelsea

Meet Niki. An active athlete who started to notice shortness of breath and persistent coughing.
"You realize your vulnerability. You realize the delicacy of life. You realize that you're not invincible."
-Niki

Meet Eric. A personal trainer who found the right specialist at the right time.
"The pulmonologist at the hospital I was at didn't know anything about aPAP. Zero."
-Eric

Hear Eric and his doctor discuss his journey with aPAP.
"Had Eric undergone blood testing for suspected autoimmune PAP, the lung biopsy and subsequent infection and hospitalization would have been avoided."
-Bruce C. Trapnell, MD
If you, like any of these patients, are struggling to find a diagnosis for respiratory symptoms that will not go away with treatment, talk to your doctor about testing for aPAP with a blood test. You can learn more and stay up to date on aPAP by signing up for updates.
Sign up for updates about aPAPTalk to your doctor if you suspect you have aPAP
Start the conversation
When is the right time to talk to your doctor? Here are some questions that may help you decide:
- Have you been experiencing persistent cough, shortness of breath, and/or fatigue, and your condition doesn’t get better with treatment?
- Did your doctor mention that your last computerized tomography (CT) scan was abnormal?
- Are your daily activities, like walking to the mailbox or up the stairs, becoming harder?
While talking to your doctor about this may feel overwhelming, it doesn’t have to be. We’ve put together a few tips to help guide the conversation with your doctor.
- Make a list of symptoms and tests that you’ve had done so far. Having this to reference will make it easier to start the conversation.
- Consider bringing a family member for support.
- Take notes during your appointment and don’t be afraid to ask questions.
Find a doctor
Results are provided by MediFind. Savara Inc. does not endorse or recommend any specific healthcare provider. Neither Savara nor MediFind have paid, or received payment from, healthcare providers for inclusion in this free tool. Search results may not include a comprehensive list of every doctor in your area.
The information provided by MediFind is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment, and does not constitute medical or other professional advice. You assume full responsibility for how you choose to use this information. Your selection of a healthcare provider is your sole responsibility and is an important decision that should be undertaken with care and discussed with your doctor.
Here are a few resources that can help you find more
information about PAP
The PAP Foundation
The PAP Foundation is a nonprofit patient advocacy organization dedicated to finding a cure and to improving the lives of those affected by pulmonary alveolar proteinosis (PAP). Through advocacy and collaboration, they promote research on PAP and provide information and support for PAP patients, healthcare professionals, and the public.
National Organization for Rare Disorders (NORD)
NORD builds community and creates a lasting impact by improving the health and well-being of people with rare diseases by driving advances in care, research, and policy. Their website includes a Pulmonary Alveolar Proteinosis Rare Disease Report and Video describing signs and symptoms, diagnosis, standard therapies, and more.
PAP Alliance
The PAP Alliance unites patients, families, clinicians, and researchers to support, inform, and fight for better outcomes. Their mission is to empower patients and families affected by PAP through education, support, and strong community. They have an education hub with resources, as well as an online forum and support groups.
American Lung Association
Founded more than 120 years ago, the American Lung Association is the leading organization working to save lives by improving lung disease through education, advocacy, and research. They have a section of their website dedicated to disease information about pulmonary alveolar proteinosis, including symptoms and diagnosis, treatment and management, and information for the newly diagnosed.
Want to learn more about aPAP? Sign up for updates.

“I think the biggest thing that you can do as someone that's new, in trying to seek a diagnosis, is stand up for yourself. You are your only advocate.”
— Kelsea